Nursing care management in substitutive renal therapy in patients with COVID-19: integrative review
Cícero Damon Carvalho-de Alencar1, Valéria de Souza-Araújo2, Maria Leni Alves-Silva2, Glauberto da Silva- Quirino1, Antonio Germane Alves Pinto1
1 Department of Nursing. Regional University of Cariri. Brazil
2 Cariri Regional Hospital. Brazil
https://doi.org/10.37551/S2254-28842023021
Como citar este artículo:
Carvalho-de Alencar CD, de Souza-Araújo V, Alves-Silva ML, da Silva-Quirino G, Alves-Pinto AG. Nursing care management in
substitutive renal therapy in patients with COVID-19: integrative review. Enferm Nefrol 2023;26(3):220-30 Enferm Nefrol 2023;26(3):232-9
Correspondencia:
|
Recepción: 28-10-2022
|
ABSTRACT
Introducción: Among the systems most affected by COVID-19, the renal system stands out, which leads to challenges in the management of nursing care for these patients.
Objetives: To describe the scientific evidence on nursing care management in patients diagnosed with COVID-19 undergoing Renal Replacement Therapy.
Methodology: Articles were searched in PubMed, SCOPUS, Web of Science, LILACS, BDENF, EMBASE, IBECS, CINAHL, COCHRANE LIBRARY, and Scielo databases, using the following cross-references: “renal therapy” AND “nursing care” AND “covid-19”. To systematize the searches, the Boolean operator “AND” was used. Initially, 167 primary references were identified in the selected databases/virtual library, and as a final sample, 14 articles were included.
Results: It was found that among the contributions to nursing care management in hemodialysis patient care in the context of the COVID-19 pandemic, the use of health technologies (examples: use of telehealth and the development of new protocols), development of new methods in nursing care management and continuing education are described in the literature. These tools were essential for the continuity of nursing care.
Conclusion: Among the tools used for nursing care management in the context of the pandemic of COVID-19 in hemodialysis patients, health technologies and continuing education in health are included, enabling qualified care management.
Keywords: renal replacement therapy; COVID-19; nursing.
ABSTRACT
Gestión de Cuidados de Enfermería en Terapia Renal Sustitutiva en Pacientes con COVID-19: Revisión Integradora
Introducción: Entre los sistemas más afectados por la pandemia COVID-19, destaca el sistema renal, circunstancia que conlleva desafíos en la gestión de cuidados de enfermería en los pacientes.
Objetivos: Describir la evidencia científica sobre la gestión de cuidados de enfermería en pacientes diagnosticados con COVID-19 sometidos a terapia renal sustitutiva.
Metodología: Se buscaron artículos en las bases de datos PubMed, SCOPUS, Web Of Science, LILACS, BDENF, EMBASE, IBECS, CINAHL, COCHRANE LIBRARY y Scielo, utilizando las siguientes palabras clave cruzadas: “renal therapy” AND “nursing care” AND “covid-19”. Para sistematizar las búsquedas, se utilizó el operador booleano “AND”. Inicialmente, se identificaron 167 referencias primarias en las bases de datos seleccionadas, y como muestra final, se incluyeron 14 artículos.
Resultados: Se encontró que entre las contribuciones a la gestión de cuidados de enfermería en la atención de pacientes en hemodiálisis en el contexto de la pandemia de COVID-19, se describen el uso de tecnologías de la salud (ejemplos: el uso de telemedicina y el desarrollo de nuevos protocolos), el desarrollo de nuevos métodos en la gestión de cuidados de enfermería y la educación continua. Estas herramientas fueron esenciales para la continuidad de los cuidados de enfermería.
Conclusión: Entre las herramientas utilizadas para la gestión de cuidados de enfermería en el contexto de la pandemia de COVID-19 en pacientes en hemodiálisis, se incluyen las tecnologías de la salud y la educación continua en salud, lo que permite una gestión de cuidados calificada.
Palabras clave: terapia de renal sustitutiva; COVID-19; enfermería.
INTRODUCTION
COVID-19 can cause multisystemic infections, as well as the acute respiratory syndrome1 which, due to its transmissibility, has become a worldwide public health problem, reaching incalculable dimensions corresponding to deaths and confirmed cases in all continents2.
In this context, pre-existing kidney disease, and especially when it is classified in terminal stage, represents a risk framework for the COVID-19 virus, as well as people who have undergone kidney transplantation. These situations are more prone to more severe complications of the infection, possibly leading to death3,4.
Data indicate an incidence of 3 to 15% of acute kidney injury in people infected by SARS-CoV-2. In more clinically severe patients requiring intensive care, the renal injury rate increases to 14.5 to 50%5-7. About 20% of patients admitted to the Intensive Care Unit diagnosed with the new coronavirus require renal replacement therapy, on average 15 days after the onset of the disease7.
Acting in renal replacement therapy, nurses are a reference in caring for the population, establishing bond, trust relationship, guiding, listening and educating patients and their families. These professionals provide nursing care, detect complications that may occur during the process of renal replacement therapy, especially when the patient is clinically severe, which is the case of patients who develop kidney injury due to the new Coronavirus8.
Also, within the nurse’s performance facing the hemodialysis process, it is necessary to plan the Systematization of Nursing Care, based and centered on logical reasoning and clinical judgment to conduct and monitor the patient’s dialysis treatment during the process of becoming ill9.
Thus, research in the context of nursing care practice is necessary, considering the numerous impacts of COVID-19 on nursing care, and it is necessary that actions are applied in services, in order to improve nursing care provided to patients in renal replacement therapy diagnosed with COVID-19. From this perspective, the objective of this study was to describe the scientific evidence on nursing care management in patients diagnosed with COVID-19 undergoing renal replacement therapy.
METHODOLOGY
Design
This is an Integrative Literature Review to describe the evidence on the management of clinical nursing care in patients with a diagnosis of COVID-19 undergoing renal replacement therapy.
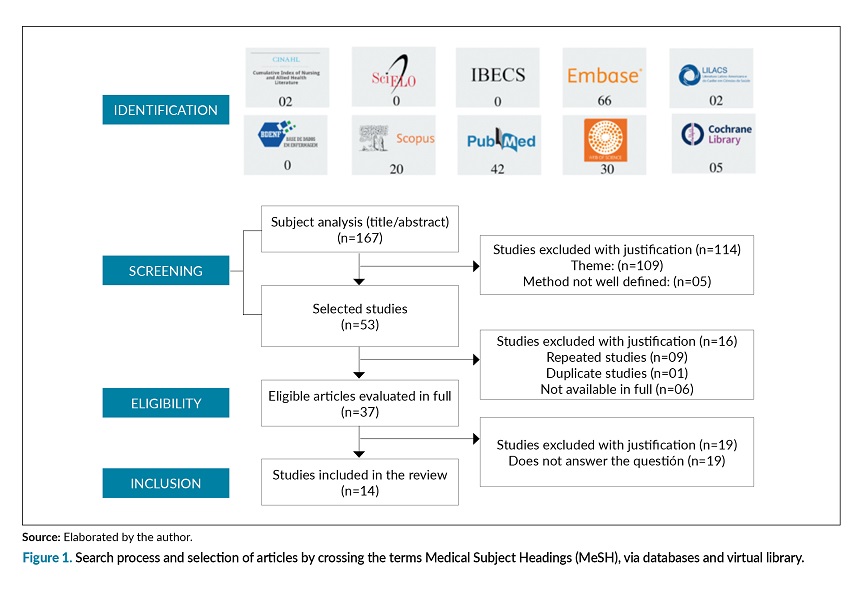
The study followed the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)10 to report the process of identification, screening, eligibility and inclusion of articles, as represented in figure 1.
The construction process followed the six steps proposed by Mendes, Silveira, and Galvão (2019)11: identification of the topic and development of the guiding question; establishment of criteria for study selection, study categorization, analysis of the studies included in the review, interpretation of results, and presentation of the review.
The operationalization of the research began with the definition of the guiding question: Which strategies identified in the literature are directed to the management of nursing care in renal replacement therapy in patients diagnosed with COVID-19?
Search method
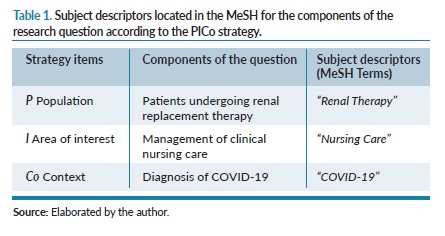
The basis of the search strategy for the primary studies was determined by the delimitation of the combined controlled descriptors based on the logical structure of the PICo strategy, which is an acronym for Problem, Interest and Context, as shown in table 1.
In a paired manner, data collection was performed from May to July 2021 in the following databases: PubMed, SCOPUS, Web Of Science, Latin American and Caribbean Literature on Health Sciences (LILACS), Nursing Database (BDENF), EMBASE, IBECS, virtual library (Scielo), Cumulative Index to Nursing and Allied Health Literature (CINAHL), COCHRANE LIBRARY.
The search in the databases occurred by crossing the Descriptors in Health Sciences (DeCS): “renal therapy” AND “nursing care” AND “covid-19”. To systematize the searches, the Boolean operator “AND” was used.
Inclusion and exclusion criteria
Inclusion criteria
The inclusion criteria were: articles available in full in Portuguese, English or Spanish.
Exclusion criteria
Studies of the type letter to the editor, dissertations, theses, repeated and duplicate studies were excluded. The analysis of references was based on publications from December 2019, justified by the emergence of the 1st case of COVID-19.
PRISMA Guideline
Initially, 167 primary references were identified in the selected databases/virtual library. After identification, the screening process began, through content analysis, which included reading the title, abstract and analysis of the adequacy to the inclusion criteria. In this process, the articles repeated among the selected ones were identified and, finally, the definitive selection of eligible references for reading in full was performed. The details of the search can be seen in figure 1.
The results of the researches of both researchers were compared, establishing agreement as to the formulation of the final sample. Initially, the studies were selected based on the title and abstract. Subsequently, the texts were carefully read in order to confirm the articles that answered the guiding question of the study.
The analysis of the results was performed from the complete reading of the articles and the extraction of data related to the theme. The results were organized and presented in tables, and the findings were interpreted and discussed critically and descriptively in light of the relevant literature.
Data extraction
For data extraction, it was performed an adaptation of the form proposed by Ursi and Galvão (2006)12, contemplating the variables year, place, language, title, indexation base, objective, methodological design and results that answer the research question. With regard to the quality of the studies (Table 2), we used the Critical Appraisal Skills Programme (CASP)13.

Summary of the results
After the selection of studies, 14 articles were included for the review, according to the established inclusion and exclusion criteria.
Ethical aspects
It is punctuated that this study dispensed with the research ethics committee’s appreciation because it is a study of review study using public domain data. It is emphasized that the ethical aspects in following the stages of the proposed review and the identification of the references used were respected.
RESULTS
Characterization of the studies included in the Review
Regarding the year of publication of the articles, it was observed a predominance of articles published in 2020, with 11 studies (79%) published in 2020 and three (21%) in 2021. Regarding the language of the manuscripts, all were published in English.
Regarding the themes addressed in the articles, an investigative approach was seen on aspects related to hemodialysis, nursing care management and strategies for coping with the pandemic, such as the use of health technologies and continuing education. Regarding the location where the studies were conducted, there was a predominance of articles from North America (N=09). The details can be seen in table 2.
Regarding the outcomes of the studies (table 3), it is observed that among the themes addressed involving the management of nursing care in the context of Renal Replacement Therapy and COVID-19, the literature discusses the team training. In view of this, taking into account the lack of knowledge of the new coronavirus, especially at the beginning of the pandemic and the challenges it imposed on the health system, the training of health professionals was one of the ways to deal with COVID-19.

In the context of health care, technologies were essential to face COVID-19, such as the development of new protocols, aiming at organizing and directing nursing care. In line with this, Continuing Education contributed directly to the fight against the pandemic, being used mainly in forms of training with the team, involving virtual discussions, online workshops, availability of training materials, videoconferences and use of telehealth technology.
DISCUSSION
Nursing Care Management in Renal Replacement Therapy
In various environments and levels of health care, the role of the nursing professional is revealed in the coordination and management of health teams and services. Currently, nursing accounts for more than half of the workforce in the health care context28.
Nursing was presented as a profession that acts on several fronts in the fight against the pandemic. However, the work of nursing has already been seen in other historical moments, whether in epidemics or catastrophes that have affected humanity. Several times, they put themselves in danger to provide health care. In COVID-19, nurses were exposed to SARS-Cov-2 in long working days29.
In health institutions, timely organizational planning was necessary in order to meet the needs of material and human resources, composition of integrated interventions and definition of various action plans due to the pandemic context. In all the processes for restructuring health services, nursing management was fundamental30,31.
From the perspective of renal replacement therapy, the nurse is the professional responsible for managing the care of patients on hemodialysis, which in turn requires knowledge and leadership, and in times of pandemic, resilience and appropriate management to meet the challenges imposed by the new coronavirus. It is urgent to ensure a qualified care with better health outcomes for patients. It is worth noting that, in a certain period of the pandemic, managers and health professionals faced a scenario of uncertainty, being the basis with scientific evidence the best reference for safe care32,33.
Among the evidence of the consequences of COVID-19, acute kidney injury is included. As a result, these patients require intensive care, so the nursing team has an important contribution in participating in the management of care to this public, given also the complications of respiratory infections linked to the kidney problem. Given this demand, it is important that nurses develop strategies aimed at patient safety, since they are responsible for managing nursing care33.
It is also noteworthy that the scenario triggered by the pandemic unveiled new forms of care, through an improved practice and supported by scientific evidence, being able to provide patient safety. Thus, nursing when implementing dialysis to a patient with COVID-19 requires preparation and understanding for the early identification of possible complications in order to mitigate adverse events in the dialysis process34.
Health technologies in the pandemic context
Due to the international public health emergency scenario, there was a need for change in the traditional care model. Healthcare organizations had to interrupt face-to-face care and invest in technological solutions to perform clinical follow-up of patients in a non-face-to-face manner35,36. An example of technology observed in the integrative review sample that allowed the continuation of care even remotely is the use of telehealth technology.
Telehealth technology played a significant role in service delivery at three points in the SARS-Cov-2 pandemic: (1) outpatient home care; (2) initial hospital outbreak of COVID-19; and (3) case recovery and treatment37,38.
In addition, there is evidence on the benefits of telehealth, such as reducing the time of care, cost / time of travel of the patient to the health service and quality of service provided. Thus, it has become a tool that enables more agile access to expert professionals39,40.
Given the scope and flexibility of technologies, such as digital technologies, which in the context of health provide innovative solutions for the provision of services, offering a range of possibilities in situations of epidemics or more serious scenarios, as experienced in the current pandemic41.
Thus, the advance of interactive technologies in the health area is considered an effective and safe option for patient care, in which it allows contact between the professional and the client. Consequently, the pandemic of COVID-19 caused a revolution in the health sector, since the imposition of the need for new strategies and adequacy of services facing the new reality42. Social vulnerability is considered a limiting condition for the population’s access to digital health technologies.
Continuing education in the COVID-19 scenario
Regarding this theme, it was found that some studies address Continuing Education as a strategy, both as a tool for coping with COVID-19, and also to improve the management of nursing care to the patient. And furthermore, reinforcing such statement, Gama and collaborators (2021)43 reinforce the need for constant updating of health professionals, considering the epidemic scenario.
An essential priority in the management of nurses in the care of the individual with COVID-19 is to provide continuous training. In this regard, the World Health Organization recommends training in health services, according to the need for technical and scientific updates44,45.
Other literature reinforces this need for training for nursing professionals who are on the front line of the pandemic, aiming at the consistent use of exposure barriers, as well as fundamental adjustments in the structure of operational flows of services and health challenges46,47.
Due to the global health crisis, it was necessary to structure Institutional Protocols, based on the Protocols of the Ministry of Health. One of the tactics used for the dissemination of information were educational actions, with the support of Continuing Education, intending the systematization of nursing care48.
For Santos and collaborators (2021)49, the implementation of Continuing Education during the pandemic was challenging, due to some factors such as keeping up with the numerous protocol updates and, along with that, the training of the multiprofessional team. Thus, this method has several potentialities, such as the propagation and continuous exchange of knowledge among health professionals.
Given the problems emerged by SARS-Cov-2 in public health worldwide, Continuing Education is an essential tool in facing the pandemic of COVID-19, with the purpose of promoting knowledge, transforming professional practice and establishing strategies for coherent assistance49.
Limitations of the study
The study is limited by presenting data with a generalist focus, not evidencing actions for the management of nursing care in Renal Replacement Therapy for specific audiences in the context of the pandemic of COVID-19.
Practical considerations
COVID-19 as other pandemics left numerous marks in society, however, the data of previous pandemics were important to project the potentiality of the new coronavirus. Thus, the data presented in this review were essential for the management of nursing care to hemodialysis patients, since health technologies and continuing education were instruments that improved nursing practice for a qualified assistance.
Based on the results of this review, in the management of nursing care for patients undergoing renal replacement therapy with COVID-19, due to the obstacles imposed by the new coronavirus, there has been a need to reorganize and develop new strategies in the global health system. Thus, among the tools used for care management are health technologies, even if not in person, in the case of telehealth.
For nursing, the technologies contributed to various aspects of the care process, such as protocols, which guide assistance and organize the service at the same time. Another important tool for the consolidation of care management in an effective way is the permanent education, which allowed the updating of health professionals, taking into account the constant discoveries about COVID-19.
Thus, such data can serve for future epidemics/pandemics, given the frequency of these phenomena. Considering the technologies and continuing education as essential tools to assist in the health-disease context, and also in the professionals’ training processes.
Conflict of interest
The authors declare that they have no potential conflicts of interest related to the content presented in the review.
Financing
The authors declare that they have not received any funding.
REFERENCES
1. Lu R, Zhao X, Li J, Niu P, Yang B, Wu H et al. Genomic characterization and epidemiology of new 2019 coronaviruses: implications for virus origins and receptor binding. The lancet [Internet]. 2020 [cited 2022 Jun 20];395(10224): 565-74. Available from: https://doi.org/10.1016/S0140-6736(20)30251-8.
2. Aspiazu MB, Bayard RB, Azcuy OH, Llerena TZ, Rodríguez EL, González LP. Función de la pesquisa activa estudiantil en el enfrentamiento a la pandemia COVID 19 en la atención primaria de salud. Rev cubana med [Internet] 2021 [cited 2023 Jun 20]; 60(2):e1660. Available from: https://revmedicina.sld.cu/index.php/med/article/view/1660/2082.
3. Gandhi RT, Lynch JB, Rio C. Mild or Moderate Covid-19. N Engl J Med [Internet]. 2020 [cited 2022 Jun 21]; 383(18): 1757-66. Available from: 10.1056/NEJMcp2009249.
4. Luigi V, Kruger T, Seikrit C, Muhlfeld AS, Kunter U, Werner C et al. Time on previous renal replacement therapy is associated with worse outcomes of COVID-19 in a regional cohort of kidney transplant and dialysis patients. Medicine [Internet]. 2021 [cited 2022 Jun 21];100(10): 1-8. Available from: 10.1097/MD.0000000000024893.
5. Cheng Y, Luo R, Wang K, Zhang M, Wang Z, Dong L et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney int [Internet]. 2020 [cited 2023 Jun 20];97(5): 829-38. Available from: 10.1016/j.kint.2020.03.005.
6. Zhang G, Hu C, Luo L, Fang F, Chen Y, Li J et al. Clinical features and short-term outcomes of 221 patients with COVID-19 in Wuhan, China. J Clin Virol [Internet]. 2020 [cited 2023 Jul 02];127:1-8. Available from: 10.1016/j.jcv.2020.104364.
7. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet [Internet]. 2020 [cited 2023 Jul 02]; 395(10229):1054-62. Available from: 10.1016/S0140-6736(20)30566-3.
8. Nigri RB, Silva RFA. Hemodiálise no contexto da Covid-19: os cuidados, o protagonismo da enfermagem e a qualidade. Rev Bras de Enferm [Internet]. 2021 [cited 2023 Jun 02];75(1):e20201077. Available from: https://doi.org/10.1590/0034-7167-2020-1077.
9. Silva AFS, Magalhães DM, Rocha PRS, Silva RF. Intervenções de Enfermagem Para Complicações Apresentadas Durante a Hemodiálise em Pacientes Críticos. Rev Enfermagem do Centro-Oeste Mineiro [Internet]. 2018 [cited 2023 May 12];8:1-9. Available from: https://doi.org/10.19175/recom.v8i0.2327.
10. Prisma. Transparente Reporting of Systematic Reviews and Meta-Analyses [cited 2022 Aug 10]. Available from: https://prisma-statement.org/.
11. Mendes KDS, Silveira RCCP, Galvão CM. Uso de gerenciador de referências bibliográficas na seleção dos estudos primários em revisão integrativa. Texto & Contexto Enfermagem [Internet] 2019 [cited 2023 May 13];28:e20170204. Available from: https://doi.org/10.1590/1980-265X-TCE-2017-0204.
12. Ursi ES, Galvão CM. Prevenção De Lesões De Pele No Perioperatório: Revisão Integrativa Da Literatura. Rev Latino Am Enfermagem [Internet]. 2006 [cited 2023 May 12]; 14(1):124-31. Available from: https://doi.org/10.1590/S0104-11692006000100017.
13. CRITICAL APPRAISAL SKILLS PROGRAMME. CASP. [cited 2023 Aug 28]. Available from: https://casp-uk.net/casp-tools-checklists/.
14. Chua HR, Laren GM, Choong LH, Chionh CY, Khoo BZ, Yeo SC. Ensuring sustainability of continuous kidney replacement therapy in the face of extraordinary demand: lessons from the COVID-19 pandemic. Am J Kidney Dis [Internet]. 2020 [cited 2023 May 13];76(3):392-400. Available from: 10.1053/j.ajkd.2020.05.008.
15. Corbett RW, Blakey S, Nitsch D, Loucaidou M, Lean A, Duncan N. Epidemiology of COVID-19 in an urban dialysis center. J Am Soc Nephrol [Internet]. 2020 [cited 2023 Jun 01];31(8):1815-23. Available from: 10.1681/ASN.2020040534.
16. Nair D, Malhotra S, Lupo D, Harbert G, Scherer JS. Challenges in communication, prognostication and dialysis decision-making in the COVID-19 pandemic: implications for interdisciplinary care during crisis settings. Curr opin nephrol hypertens [Internet]. 2021 [cited 2023 Jun 01];30(2):190-7. Available from: 10.1097/MNH.0000000000000689.
17. MitchelL KR, Bomm A, Shea BS, Shemin D, Bayliss G. Inpatient dialysis planning during the COVID-19 pandemic: a single-center experience and review of the literature. Int J Nephrol Renovasc Dis [Internet]. 2020 [cited 2023 Jun 01];13: 253-9. Available from:10.2147/IJNRD.S275075.
18. Noce E, Zorzanello M, Patel D, Kodali R. Management of COVID-19 in an Outpatient Dialysis Program. Nephrol Nurs J [Internet]. 2020 [cited 2023 May 16];47(5):423-7. Available from: 10.1177/2054358120938564.
19. Apata IW, Cobb J, Navarrete J, Bukart J, Laura P, Lea JP. COVID-19 infection control measures and outcomes in urban dialysis centers in predominantly African American communities. BMC nephrol [Internet]. 2021 [cited 2023 May 163];22(1):1-9. Available from: 10.1186/s12882-021-02281-6.
20. Yin J, Yin J, Tian Z, Li P, Chen X. Integrated management is effective in the prevention and control of COVID-19 in the blood purification center: joint efforts from multiple departments. Renal Replacement Therapy [Internet]. 2021 [cited 2023 May 16];7(1):1-5. Available from: 10.1186/s41100-021-00334-y.
21. Naamani Z, Gorley K, Nobre H, Santin O, Maqbali M. Fatigue, anxiety, depression and sleep quality in patients undergoing haemodialysis. BMC nephrol [Internet]. 2021 [cited 2023 Jun 20];22(1):1-8. Available from: 10.1186/s12882-021-02349-3.
22. Lang CN, Zotzmann V, Schmid B, Berchtold-Herz M, Utzolino S, Paul B et al. Intensive care resources and 60-day survival of critically-Ill COVID-19 patients. Cureus [Internet]. 2021 [cited 2023 Jun 13];12(2):e13210. Available from: 10.7759/cureus.13210.
23. Wasserman E, Toal M, Nellis M, Traube C, Joyce C, Finkelstein R et al. Rapid transition of a PICU space and staff to adult coronavirus disease 2019 ICU care. Pediatr Crit Care Med [Internet]. 2021 [cited 2023 Jun 13];22(1):50-5. Available from: 10.1097/PCC.0000000000002597.
24. Lew SQ, Wallace EL, Srivatana V, Warady BA, Watnick S, Hood J et al. Telehealth for home dialysis in COVID-19 and beyond: a perspective from the American Society of Nephrology COVID-19 Home Dialysis Subcommittee. Am J Kidney Dis [Internet]. 2021 [cited 2023 Jun 13];77(1):142-8. Available from:10.1053/j.ajkd.2020.09.005.
25. Brickman D, Greenway A, Sobocinski K, Thai H, Turick A, Xuereb K et al. Rapid critical care training of nurses in the surge response to the coronavirus pandemic. Am J Crit Care [Internet]. 2020 [cited 2023 Jun 13];29(5):104-7. Available from: 10.4037/ajcc2020142.
26. Ehmann MR, Zink E, Levin AB, Suarez J, Belcher HME, BiddisonELD et al. Operational recommendations for scarce resource allocation in a public health crisis. Chest [Internet]. 2021 [cited 2023 May 16];159(3):1076-83. Available from: 10.1016/j.chest.2020.09.246.
27. Bruyneel A, Gallani MC, Tack J, Hondt A, Canipel S, Stéphane F et al. Impact of COVID-19 on nursing time in intensive care units in Belgium. Intensive Crit Care Nurs [Internet]. 2021 [cited 2023 May 26];62:1-6. Available from: 10.1016/j.iccn.2020.102967.
28. World Health Organization, State of the world’s nursing 2020: investing in education, jobs and leadership. [cited 2023 Mar 13]. Available from: https://apps.who.int/iris/handle/10665/331677.
29. World Health Organization, COVID-19: Occupational health and safety for health workers: interim guidance. [cited 2023 Mar 05]. Available from: https://www.who.int/publications/i/item/coronavirus-disease-(covid-19)-outbreak-rights-roles-and-responsibilities-of-health-workers-including-key-considerations-for-occupational-safety-and-health.
30. Almeida JÁ. Medicina Interna do Centro Hospitalar Universitário S. João na Pandemia COVID-19. Medicina Interna [Internet]. 2020 [cited 2023 May 26];1-6. Available from: https://doi.org/10.24950/rspmi/COVID19/J.Almeida/CHUSJOAOS/2020.
31. Silva JMAV, Ribeiro OMPL, Santos MR, Faria ACA, Monteiro MAJ, Vandresen L. Planejamento organizacional no contexto de pandemia por COVID-19: implicações para a gestão em enfermagem. J Health NPEPS [Internet]. 2020 [cited 2023 Jun 20];5(1):1-18. Available from: https://pesquisa.bvsalud.org/portal/resource/pt/biblio-1103674.
32. Kruk ME, Myers M, Varpilah ST, Dahn BT. What is a resilient health system? Lessons from Ebola. Lancet [Internet]. 2015 [cited 2023 May 28];385(9980):1910-2. Available from: 10.1016/S0140-6736(15)60755-3.
33. Queiroz JS, Marques PF. Gerenciamento de enfermagem no enfrentamento da COVID-19 nos serviços de hemodiálise. Enferm Foco [Internet]. 2020 [cited 2023 May 28];11(1):196-8. Available from: https://doi.org/10.21675/2357-707X.2020.v11.n1.ESP.3536.
34. Pennafort VPS, Mendonça AEO, Nunes VMA. Cuidado do paciente hospitalizado com COVID-19 em hemodiálise: relato de experiência. Archives of Health [Internet]. 2021 [cited 2023 Jun 20];2(4):1352-5. Available from: https://ojs.latinamericanpublicacoes.com.br/ojs/index.php/ah/article/view/644.
35. Greenhalgh, T, Koh GCH, Car J. Covid-19: a remote assessment in primary care. Bmj [Internet]. 2020 [cited 2023 May 28];368:1-5. Available from: https://doi.org/10.1136/bmj.m1182.
36. Fagherazzi G, Goetzinger C, Rashid MA, Aguayo GA, Huiart L. Digital health strategies to fight COVID-19 worldwide: challenges, recommendations, and a call for papers. J Med Internet Res [Internet]. 2020 [cited 2023 Jun 19];22(6): p.e1928. Available from: doi:10.2196/19284.
37. Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc [Internet]. 2020 [cited 2023 Jun 19];27(6):957-62. Available from: 10.1093/jamia/ocaa067.
38. Sarbadhikari S, Sarbadhikari SN. The global experience of digital health interventions in COVID-19 management. Indian J public health [Internet]. 2020 [cited 2023 Jun 19];64(6):117-24. Available from: 10.4103/ijph.IJPH_457_20.
39. Toit M, Malau-Aduli B, Vangaveti V. Use of telehealth in the management of non-critical emergencies in rural or remote emergency departments: a systematic review. J telemedicine and telecare [Internet]. 2019 [cited 2023 Jun 19]; 25(1):3-16. Available from: 10.1177/1357633X17734239.
40. Caffery LJ, Farjian M, Smith AC. Telehealth interventions for reducing waiting lists and waiting times for specialist outpatient services: A scoping review. J telemed telecare [Internet]. 2016 [cited 2023 Jun 19];22(8):504-12. Available from: 10.1177/1357633X16670495.
41. Caetano R, Silva AB, Guedes ACCM, Paiva CCN, Ribeiro GR, Santos DL et al. Desafios e oportunidades para telessaúde em tempos da pandemia pela COVID-19: uma reflexão sobre os espaços e iniciativas no contexto brasileiro. Cad Saúde Pública [Internet]. 2020 [cited 2023 Jun 05];36(5):1-16. Available from: https://doi.org/10.1590/0102-311X00088920.
42. Celippi IC, Lima GS, Rossi E, Wazlawick RS, Dalmarco EM. Uma análise sobre o desenvolvimento de tecnologias digitais em saúde para o enfrentamento da COVID-19 no Brasil e no mundo. Cad Saúde Pública [Internet]. 2021 [cited 2023 Jun 02];37(3):1-12. Available from: https://doi.org/10.1590/0102-311X00243220.
43. Gama BMBM, Cruz CMA, França LM, Ferreira MR, Gomes SS, Godinho MR. Pandemia de COVID-19 e os cuidados de enfermagem aos pacientes em tratamento hemodialítico. Esc. Anna. Nery [Internet]. 2020 [cited 2023 Jun 05]; 24:1-7. Available from: https://doi.org/10.1590/2177-9465-EAN-2020-0413.
44. Bitencourt JVOV, Meschial WC, Friozon G, Biffi P, Souza JB, Maestri E. Protagonismo do enfermeiro na estruturação e gestão de uma unidade específica para covid-19. Texto & Contexto-Enfermagem [Internet]. 2020 [cited 2023 Jun 05];29:e20200213. Available from: https://doi.org/10.1590/1980-265X-TCE-2020-0213.
45. World Health Organization. Health Care Readiness. [cited 2023 Mar 28]. Available from: https://www.who.int/teams/health-care-readiness/covid-19.
46. Reis LM, Lago PN, Carvalho AHS, Nobre VNN, Guimarães APR. Atuação da enfermagem no cenário da pandemia COVID-19. Nursing (São Paulo) [Internet]. 2020 [cited 2023 Jun 05];23(269):4765-72. Available from: https://doi.org/10.36489/nursing.2020v23i269p4765-4772.
47. Feliciano AB, Fortuna CM, Silva MV, Santos KS, Araujo PN, Franceschini ABC. A pandemia de covid-19 e a educação permanente em saúde. Cadernos da Pedagogia [Internet]. 2020 [cited 2023 Jun 20];14(29):120-35. Available from: https://www.cadernosdapedagogia.ufscar.br/index.php/cp/article/view/1457.
48. PERNAMBUCO. Secretaria de Saúde – Segurança do Paciente: recomendações aos Núcleos de Segurança do Paciente no Enfrentamento da COVID-19. Pernambuco, 2020. 102f.
49. Santos JLS, Santana FA, Serafim CS, Freitas LR, Oliveira WLS, Melo MVS et al. Enfrentamento a covid-19: importância da educação permanente em serviços de saúde. Revista Eletrônica Acervo Enfermagem [Internet]. 2021 [cited 2023 Jun 05];13:1-10. Available from: https://doi.org/10.25248/reaenf.e8669.2021.
Este artículo se distribuye bajo una Licencia Creative Commons Atribución–NoComercial 4.0 Internacional.
https://creativecommons.org/licenses/by-nc/4.0/
